Uni-compartmental knee replacement (UKR), known as partial knee replacement, is a surgical intervention focused on replacing solely the impaired surfaces of one compartment of the knee (Medial or Lateral), typically caused by severe arthritis. During this procedure, metal and plastic implants are employed to resurface the damaged cartilage and underlying bones in a specific area of the knee.
Partial knee replacement (UKR) is typically recommended for individuals who meet the following criteria:
Advanced arthritis localized to one side of the knee, either the medial (inner) or the lateral (outer) side Intact ligaments, good mechanical stability, and a satisfactory range of motion in the knee Healthy cartilage and bones in the non-affected compartments Have exhausted conservative (non-surgical) treatments, such as lifestyle adjustments, pain relief medications, knee exercises, weight management, cartilage supplements, and lubrication injections Experience worsening symptoms despite the aforementioned measures, or encounter significant adverse effects from medications.
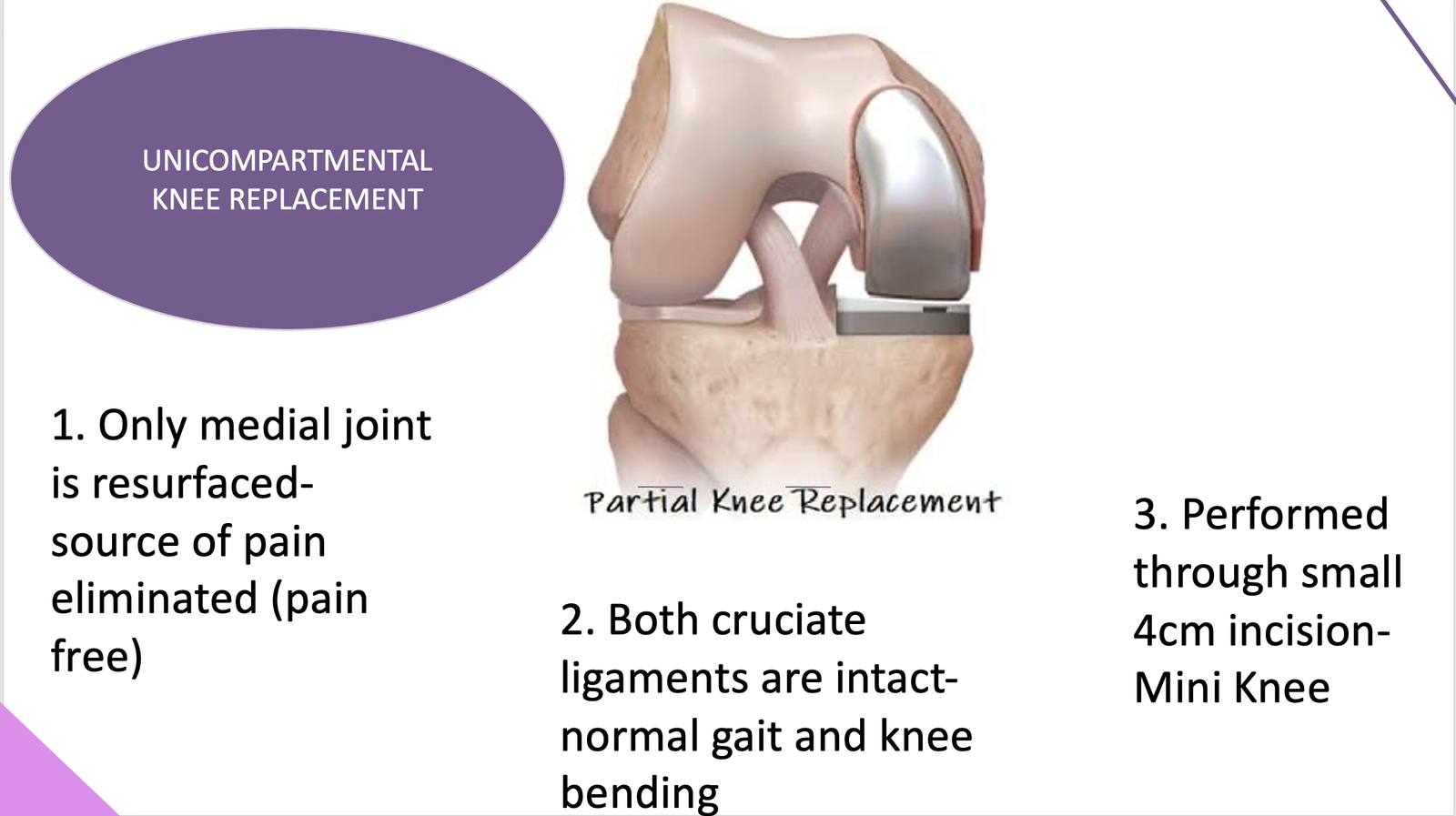
Uni-compartmental knee replacement surgery, when performed on carefully selected patients, provides the following benefits:
 Both cruciate ligaments are intact- normal gait and knee bending
Both cruciate ligaments are intact- normal gait and knee bending
 Bone and tissue preserving
Bone and tissue preserving
 Performed through small 4cm incision- Mini Knee Replacement
Performed through small 4cm incision- Mini Knee Replacement
 Decreased tissue trauma, resulting in less pain and minimal blood loss
Decreased tissue trauma, resulting in less pain and minimal blood loss
 Quicker recovery period
Quicker recovery period
 Shorter hospital stay, typically 1 to 2 days only
Shorter hospital stay, typically 1 to 2 days only
 Enhanced natural feel of the knee and improved range of motion
Enhanced natural feel of the knee and improved range of motion
The following conditions serve as contraindications for a partial knee replacement:
 Active or suspected infection in or around the knee joint
Active or suspected infection in or around the knee joint
 Inflammatory arthritis such as Rheumatoid arthritis
Inflammatory arthritis such as Rheumatoid arthritis
 Significant knee stiffness
Significant knee stiffness
 Major bone deformities altering mechanical alignment
Major bone deformities altering mechanical alignment
 Neuro-muscular disorders affecting patient mobility and balance
Neuro-muscular disorders affecting patient mobility and balance
 Obesity
Obesity
 Advanced patellofemoral arthritis
Advanced patellofemoral arthritis
 Unstable knee due to ligament insufficiency
Unstable knee due to ligament insufficiency
 Untreated damage within the non-affected compartment
Untreated damage within the non-affected compartment
The steps involved in a partial knee replacement surgery are as follows:
 The procedure may be performed under epidural, spinal, or general anesthesia. Epidural anesthesia is preferred as it can provide up to 48 hours of post-operative pain relief and facilitate faster progress in physiotherapy.
The procedure may be performed under epidural, spinal, or general anesthesia. Epidural anesthesia is preferred as it can provide up to 48 hours of post-operative pain relief and facilitate faster progress in physiotherapy.
 The knee is prepared with a sterile solution to prevent infection, and a tourniquet is inflated to minimize blood loss during the operation.
The knee is prepared with a sterile solution to prevent infection, and a tourniquet is inflated to minimize blood loss during the operation.
 A small incision, typically 3-4 inches in length, is made alongside the patella (kneecap) to expose the knee joint.
A small incision, typically 3-4 inches in length, is made alongside the patella (kneecap) to expose the knee joint.
 The joint is carefully examined to confirm that arthritis is primarily confined to one side of the knee and that other compartments are healthy.
The joint is carefully examined to confirm that arthritis is primarily confined to one side of the knee and that other compartments are healthy.
 If significant cartilage damage is found on the under-surface of the patella or on the opposite side of the knee, a partial knee replacement may not provide effective pain relief. In such cases, a traditional total knee replacement may be necessary.
If significant cartilage damage is found on the under-surface of the patella or on the opposite side of the knee, a partial knee replacement may not provide effective pain relief. In such cases, a traditional total knee replacement may be necessary.
 Specialized alignment tools and cutting jigs are used to remove enough bone from the femur and tibia to accommodate the partial knee replacement implants. Proper sizing and alignment of the implants are crucial for optimal post-operative function and pain relief.
Specialized alignment tools and cutting jigs are used to remove enough bone from the femur and tibia to accommodate the partial knee replacement implants. Proper sizing and alignment of the implants are crucial for optimal post-operative function and pain relief.
 Trial implants are temporarily placed without bone cement to assess their fit against the cut bony surfaces. Factors such as limb alignment, ligament balance, stability, and range of motion are evaluated before final implantation.
Trial implants are temporarily placed without bone cement to assess their fit against the cut bony surfaces. Factors such as limb alignment, ligament balance, stability, and range of motion are evaluated before final implantation.
 Once the appropriate sizing and fit are confirmed, the definitive femoral and tibial implants are cemented into place using bone cement. The plastic insert between the implants may be of the mobile bearing or fixed bearing type, depending on pre-operative planning and surgeon preference.
Once the appropriate sizing and fit are confirmed, the definitive femoral and tibial implants are cemented into place using bone cement. The plastic insert between the implants may be of the mobile bearing or fixed bearing type, depending on pre-operative planning and surgeon preference.
 The average duration of partial knee replacement surgery is approximately 50 to 60 minutes.
The average duration of partial knee replacement surgery is approximately 50 to 60 minutes.
 After surgery, patients are allowed to eat and drink within 2 to 3 hours. They are closely monitored in the recovery room and then transferred to their ward bed once stable, typically staying in the recovery ward for 1 to 2 hours.
After surgery, patients are allowed to eat and drink within 2 to 3 hours. They are closely monitored in the recovery room and then transferred to their ward bed once stable, typically staying in the recovery ward for 1 to 2 hours.
 Epidural anesthesia is maintained post-surgery for 24 to 48 hours. If there's breakthrough pain, intravenous paracetamol and/or diclofenac injections are administered for the first 24 hours, which can later be switched to oral painkillers. Regular oral painkillers are taken for the initial 5 to 7 days, then as needed.
Epidural anesthesia is maintained post-surgery for 24 to 48 hours. If there's breakthrough pain, intravenous paracetamol and/or diclofenac injections are administered for the first 24 hours, which can later be switched to oral painkillers. Regular oral painkillers are taken for the initial 5 to 7 days, then as needed.
 Additional intravenous antibiotic doses are given at 8-hour intervals. Blood samples are taken the following morning to assess hemoglobin, urea, creatine, and electrolyte levels. Iron supplements are initiated if hemoglobin levels are low.
Additional intravenous antibiotic doses are given at 8-hour intervals. Blood samples are taken the following morning to assess hemoglobin, urea, creatine, and electrolyte levels. Iron supplements are initiated if hemoglobin levels are low.
 Patients are provided with ice packs regularly to reduce knee swelling and manage pain. They're encouraged to move their toes and ankles once the anesthesia wears off and can start straight leg raises if tolerated. Weight-bearing with assistance from a walker or crutches can begin the same day or the next morning. Patients are trained to perform daily activities like getting in and out of bed, using the toilet, stairs, and sitting in a chair. Range of motion knee exercises are introduced gradually.
Patients are provided with ice packs regularly to reduce knee swelling and manage pain. They're encouraged to move their toes and ankles once the anesthesia wears off and can start straight leg raises if tolerated. Weight-bearing with assistance from a walker or crutches can begin the same day or the next morning. Patients are trained to perform daily activities like getting in and out of bed, using the toilet, stairs, and sitting in a chair. Range of motion knee exercises are introduced gradually.
 Blood-thinning medications are administered daily during the hospital stay and continued orally for two weeks afterward. Once patients are safely mobile and relatively pain-free, they can be discharged home on the 2nd or 3rd day after surgery, with dressings changed before discharge. The new dressings remain undisturbed for two weeks until suture removal. Patients can resume normal bathing after suture removal, with precautions to keep the wound dry.
Blood-thinning medications are administered daily during the hospital stay and continued orally for two weeks afterward. Once patients are safely mobile and relatively pain-free, they can be discharged home on the 2nd or 3rd day after surgery, with dressings changed before discharge. The new dressings remain undisturbed for two weeks until suture removal. Patients can resume normal bathing after suture removal, with precautions to keep the wound dry.
 Normal breakfast and diet are allowed from the day following surgery, with a focus on healthy foods including green leafy vegetables and fruits. Vitamins and iron supplements may be prescribed if necessary.
Normal breakfast and diet are allowed from the day following surgery, with a focus on healthy foods including green leafy vegetables and fruits. Vitamins and iron supplements may be prescribed if necessary.
 Physiotherapy is crucial for the first 4 to 6 weeks post-surgery and may continue for 2 to 3 months. This can be done at the hospital on an outpatient basis or through home sessions supervised by an experienced physiotherapist. Ice packs are used regularly for 4 to 6 weeks post-discharge. Most patients experience pain relief and are able to walk unaided within 4 to 6 weeks after partial knee replacement.
Physiotherapy is crucial for the first 4 to 6 weeks post-surgery and may continue for 2 to 3 months. This can be done at the hospital on an outpatient basis or through home sessions supervised by an experienced physiotherapist. Ice packs are used regularly for 4 to 6 weeks post-discharge. Most patients experience pain relief and are able to walk unaided within 4 to 6 weeks after partial knee replacement.
 Office work can typically resume after 2 to 3 weeks, and car driving by the 4th postoperative week. Patients are encouraged to remain active with activities like walking, swimming, cycling, and light tennis, but high-impact activities like jogging or running are not advised and should be avoided.
Office work can typically resume after 2 to 3 weeks, and car driving by the 4th postoperative week. Patients are encouraged to remain active with activities like walking, swimming, cycling, and light tennis, but high-impact activities like jogging or running are not advised and should be avoided.
Uni-compartmental knee replacement is a remarkably successful procedure when performed on carefully chosen patients. Over time, advancements in prosthetic designs and precise instrumentation have enhanced the surgical process, allowing for precise implantation through minimal incisions. The long-term survival rates at 10 to 12 years post-surgery range between 95 to 98%, regardless of whether the procedure involves mobile bearing or fixed bearing implants. Patients typically experience freedom of movement without pain, enabling them to lead active and independent lives. Furthermore, their knees often feel nearly normal with a satisfactory range of motion.
The potential risks and complications following uni-compartmental (partial) knee replacement include:
 General anesthesia risks such as allergic reactions to medications and breathing difficulties.
General anesthesia risks such as allergic reactions to medications and breathing difficulties.
 Surgical risks such as blood clots in the legs (deep vein thrombosis) that may lead to pulmonary embolism, infections in various body areas including the lungs, urinary tract, and chest, bleeding, and fractures around the implants.
Surgical risks such as blood clots in the legs (deep vein thrombosis) that may lead to pulmonary embolism, infections in various body areas including the lungs, urinary tract, and chest, bleeding, and fractures around the implants.
 Specific complications related to UKR such as infection of the knee joint, wear of the artificial joint, loosening of the artificial joint over time, dislocation of the mobile bearing, progression of inflammatory synovial disease (lipoma arborescens), knee stiffness, and rare allergic reactions to the artificial joint.
Specific complications related to UKR such as infection of the knee joint, wear of the artificial joint, loosening of the artificial joint over time, dislocation of the mobile bearing, progression of inflammatory synovial disease (lipoma arborescens), knee stiffness, and rare allergic reactions to the artificial joint.
 Additionally, there's a risk of injury to nerves, blood vessels, or surrounding knee ligaments during surgery.
Additionally, there's a risk of injury to nerves, blood vessels, or surrounding knee ligaments during surgery.
 There's also a possibility of needing revision surgery in the future for various reasons, including the progression of arthritis in the unaffected knee compartments.
There's also a possibility of needing revision surgery in the future for various reasons, including the progression of arthritis in the unaffected knee compartments.
 Patients with a prosthesis, like an artificial joint, should take precautions against infection by carrying a medical identification card indicating the presence of the prosthesis. Antibiotics may be necessary before dental procedures or other invasive medical interventions.
Patients with a prosthesis, like an artificial joint, should take precautions against infection by carrying a medical identification card indicating the presence of the prosthesis. Antibiotics may be necessary before dental procedures or other invasive medical interventions.
Uni-compartmental knee replacement (UKR), known as partial knee replacement, is a surgical intervention focused on replacing solely the impaired surfaces of one compartment of the knee (Medial or Lateral), typically caused by severe arthritis. During this procedure, metal and plastic implants are employed to resurface the damaged cartilage and underlying bones in a specific area of the knee.
Partial knee replacement (UKR) is typically recommended for individuals who meet the following criteria:
Advanced arthritis localized to one side of the knee, either the medial (inner) or the lateral (outer) side Intact ligaments, good mechanical stability, and a satisfactory range of motion in the knee Healthy cartilage and bones in the non-affected compartments Have exhausted conservative (non-surgical) treatments, such as lifestyle adjustments, pain relief medications, knee exercises, weight management, cartilage supplements, and lubrication injections Experience worsening symptoms despite the aforementioned measures, or encounter significant adverse effects from medications.
Uni-compartmental knee replacement surgery, when performed on carefully selected patients, provides the following benefits:
 Both cruciate ligaments are intact- normal gait and knee bending
Both cruciate ligaments are intact- normal gait and knee bending
 Bone and tissue preserving
Bone and tissue preserving
 Performed through small 4cm incision- Mini Knee Replacement
Performed through small 4cm incision- Mini Knee Replacement
 Decreased tissue trauma, resulting in less pain and minimal blood loss
Decreased tissue trauma, resulting in less pain and minimal blood loss
 Quicker recovery period
Quicker recovery period
 Shorter hospital stay, typically 1 to 2 days only
Shorter hospital stay, typically 1 to 2 days only
 Enhanced natural feel of the knee and improved range of motion
Enhanced natural feel of the knee and improved range of motion
The following conditions serve as contraindications for a partial knee replacement:
 Active or suspected infection in or around the knee joint
Active or suspected infection in or around the knee joint
 Inflammatory arthritis such as Rheumatoid arthritis
Inflammatory arthritis such as Rheumatoid arthritis
 Significant knee stiffness
Significant knee stiffness
 Major bone deformities altering mechanical alignment
Major bone deformities altering mechanical alignment
 Neuro-muscular disorders affecting patient mobility and balance
Neuro-muscular disorders affecting patient mobility and balance
 Obesity
Obesity
 Advanced patellofemoral arthritis
Advanced patellofemoral arthritis
 Unstable knee due to ligament insufficiency
Unstable knee due to ligament insufficiency
 Untreated damage within the non-affected compartment
Untreated damage within the non-affected compartment
The steps involved in a partial knee replacement surgery are as follows:
 The procedure may be performed under epidural, spinal, or general anesthesia. Epidural anesthesia is preferred as it can provide up to 48 hours of post-operative pain relief and facilitate faster progress in physiotherapy.
The procedure may be performed under epidural, spinal, or general anesthesia. Epidural anesthesia is preferred as it can provide up to 48 hours of post-operative pain relief and facilitate faster progress in physiotherapy.
 The knee is prepared with a sterile solution to prevent infection, and a tourniquet is inflated to minimize blood loss during the operation.
The knee is prepared with a sterile solution to prevent infection, and a tourniquet is inflated to minimize blood loss during the operation.
 A small incision, typically 3-4 inches in length, is made alongside the patella (kneecap) to expose the knee joint.
A small incision, typically 3-4 inches in length, is made alongside the patella (kneecap) to expose the knee joint.
 The joint is carefully examined to confirm that arthritis is primarily confined to one side of the knee and that other compartments are healthy.
The joint is carefully examined to confirm that arthritis is primarily confined to one side of the knee and that other compartments are healthy.
 If significant cartilage damage is found on the under-surface of the patella or on the opposite side of the knee, a partial knee replacement may not provide effective pain relief. In such cases, a traditional total knee replacement may be necessary.
If significant cartilage damage is found on the under-surface of the patella or on the opposite side of the knee, a partial knee replacement may not provide effective pain relief. In such cases, a traditional total knee replacement may be necessary.
 Specialized alignment tools and cutting jigs are used to remove enough bone from the femur and tibia to accommodate the partial knee replacement implants. Proper sizing and alignment of the implants are crucial for optimal post-operative function and pain relief.
Specialized alignment tools and cutting jigs are used to remove enough bone from the femur and tibia to accommodate the partial knee replacement implants. Proper sizing and alignment of the implants are crucial for optimal post-operative function and pain relief.
 Trial implants are temporarily placed without bone cement to assess their fit against the cut bony surfaces. Factors such as limb alignment, ligament balance, stability, and range of motion are evaluated before final implantation.
Trial implants are temporarily placed without bone cement to assess their fit against the cut bony surfaces. Factors such as limb alignment, ligament balance, stability, and range of motion are evaluated before final implantation.
 Once the appropriate sizing and fit are confirmed, the definitive femoral and tibial implants are cemented into place using bone cement. The plastic insert between the implants may be of the mobile bearing or fixed bearing type, depending on pre-operative planning and surgeon preference.
Once the appropriate sizing and fit are confirmed, the definitive femoral and tibial implants are cemented into place using bone cement. The plastic insert between the implants may be of the mobile bearing or fixed bearing type, depending on pre-operative planning and surgeon preference.
 The average duration of partial knee replacement surgery is approximately 50 to 60 minutes.
The average duration of partial knee replacement surgery is approximately 50 to 60 minutes.
 After surgery, patients are allowed to eat and drink within 2 to 3 hours. They are closely monitored in the recovery room and then transferred to their ward bed once stable, typically staying in the recovery ward for 1 to 2 hours.
After surgery, patients are allowed to eat and drink within 2 to 3 hours. They are closely monitored in the recovery room and then transferred to their ward bed once stable, typically staying in the recovery ward for 1 to 2 hours.
 Epidural anesthesia is maintained post-surgery for 24 to 48 hours. If there's breakthrough pain, intravenous paracetamol and/or diclofenac injections are administered for the first 24 hours, which can later be switched to oral painkillers. Regular oral painkillers are taken for the initial 5 to 7 days, then as needed.
Epidural anesthesia is maintained post-surgery for 24 to 48 hours. If there's breakthrough pain, intravenous paracetamol and/or diclofenac injections are administered for the first 24 hours, which can later be switched to oral painkillers. Regular oral painkillers are taken for the initial 5 to 7 days, then as needed.
 Additional intravenous antibiotic doses are given at 8-hour intervals. Blood samples are taken the following morning to assess hemoglobin, urea, creatine, and electrolyte levels. Iron supplements are initiated if hemoglobin levels are low.
Additional intravenous antibiotic doses are given at 8-hour intervals. Blood samples are taken the following morning to assess hemoglobin, urea, creatine, and electrolyte levels. Iron supplements are initiated if hemoglobin levels are low.
 Patients are provided with ice packs regularly to reduce knee swelling and manage pain. They're encouraged to move their toes and ankles once the anesthesia wears off and can start straight leg raises if tolerated. Weight-bearing with assistance from a walker or crutches can begin the same day or the next morning. Patients are trained to perform daily activities like getting in and out of bed, using the toilet, stairs, and sitting in a chair. Range of motion knee exercises are introduced gradually.
Patients are provided with ice packs regularly to reduce knee swelling and manage pain. They're encouraged to move their toes and ankles once the anesthesia wears off and can start straight leg raises if tolerated. Weight-bearing with assistance from a walker or crutches can begin the same day or the next morning. Patients are trained to perform daily activities like getting in and out of bed, using the toilet, stairs, and sitting in a chair. Range of motion knee exercises are introduced gradually.
 Blood-thinning medications are administered daily during the hospital stay and continued orally for two weeks afterward. Once patients are safely mobile and relatively pain-free, they can be discharged home on the 2nd or 3rd day after surgery, with dressings changed before discharge. The new dressings remain undisturbed for two weeks until suture removal. Patients can resume normal bathing after suture removal, with precautions to keep the wound dry.
Blood-thinning medications are administered daily during the hospital stay and continued orally for two weeks afterward. Once patients are safely mobile and relatively pain-free, they can be discharged home on the 2nd or 3rd day after surgery, with dressings changed before discharge. The new dressings remain undisturbed for two weeks until suture removal. Patients can resume normal bathing after suture removal, with precautions to keep the wound dry.
 Normal breakfast and diet are allowed from the day following surgery, with a focus on healthy foods including green leafy vegetables and fruits. Vitamins and iron supplements may be prescribed if necessary.
Normal breakfast and diet are allowed from the day following surgery, with a focus on healthy foods including green leafy vegetables and fruits. Vitamins and iron supplements may be prescribed if necessary.
 Physiotherapy is crucial for the first 4 to 6 weeks post-surgery and may continue for 2 to 3 months. This can be done at the hospital on an outpatient basis or through home sessions supervised by an experienced physiotherapist. Ice packs are used regularly for 4 to 6 weeks post-discharge. Most patients experience pain relief and are able to walk unaided within 4 to 6 weeks after partial knee replacement.
Physiotherapy is crucial for the first 4 to 6 weeks post-surgery and may continue for 2 to 3 months. This can be done at the hospital on an outpatient basis or through home sessions supervised by an experienced physiotherapist. Ice packs are used regularly for 4 to 6 weeks post-discharge. Most patients experience pain relief and are able to walk unaided within 4 to 6 weeks after partial knee replacement.
 Office work can typically resume after 2 to 3 weeks, and car driving by the 4th postoperative week. Patients are encouraged to remain active with activities like walking, swimming, cycling, and light tennis, but high-impact activities like jogging or running are not advised and should be avoided.
Office work can typically resume after 2 to 3 weeks, and car driving by the 4th postoperative week. Patients are encouraged to remain active with activities like walking, swimming, cycling, and light tennis, but high-impact activities like jogging or running are not advised and should be avoided.
Uni-compartmental knee replacement is a remarkably successful procedure when performed on carefully chosen patients. Over time, advancements in prosthetic designs and precise instrumentation have enhanced the surgical process, allowing for precise implantation through minimal incisions. The long-term survival rates at 10 to 12 years post-surgery range between 95 to 98%, regardless of whether the procedure involves mobile bearing or fixed bearing implants. Patients typically experience freedom of movement without pain, enabling them to lead active and independent lives. Furthermore, their knees often feel nearly normal with a satisfactory range of motion.
The potential risks and complications following uni-compartmental (partial) knee replacement include:
 General anesthesia risks such as allergic reactions to medications and breathing difficulties.
General anesthesia risks such as allergic reactions to medications and breathing difficulties.
 Surgical risks such as blood clots in the legs (deep vein thrombosis) that may lead to pulmonary embolism, infections in various body areas including the lungs, urinary tract, and chest, bleeding, and fractures around the implants.
Surgical risks such as blood clots in the legs (deep vein thrombosis) that may lead to pulmonary embolism, infections in various body areas including the lungs, urinary tract, and chest, bleeding, and fractures around the implants.
 Specific complications related to UKR such as infection of the knee joint, wear of the artificial joint, loosening of the artificial joint over time, dislocation of the mobile bearing, progression of inflammatory synovial disease (lipoma arborescens), knee stiffness, and rare allergic reactions to the artificial joint.
Specific complications related to UKR such as infection of the knee joint, wear of the artificial joint, loosening of the artificial joint over time, dislocation of the mobile bearing, progression of inflammatory synovial disease (lipoma arborescens), knee stiffness, and rare allergic reactions to the artificial joint.
 Additionally, there's a risk of injury to nerves, blood vessels, or surrounding knee ligaments during surgery.
Additionally, there's a risk of injury to nerves, blood vessels, or surrounding knee ligaments during surgery.
 There's also a possibility of needing revision surgery in the future for various reasons, including the progression of arthritis in the unaffected knee compartments.
There's also a possibility of needing revision surgery in the future for various reasons, including the progression of arthritis in the unaffected knee compartments.
 Patients with a prosthesis, like an artificial joint, should take precautions against infection by carrying a medical identification card indicating the presence of the prosthesis. Antibiotics may be necessary before dental procedures or other invasive medical interventions.
Patients with a prosthesis, like an artificial joint, should take precautions against infection by carrying a medical identification card indicating the presence of the prosthesis. Antibiotics may be necessary before dental procedures or other invasive medical interventions.
Address
8/92, Sector 8, Ismailganj, Indira Nagar, Lucknow, Uttar Pradesh 226016
Monday to Friday
10am - 8pm
Appoinments
+91 - 8840223370