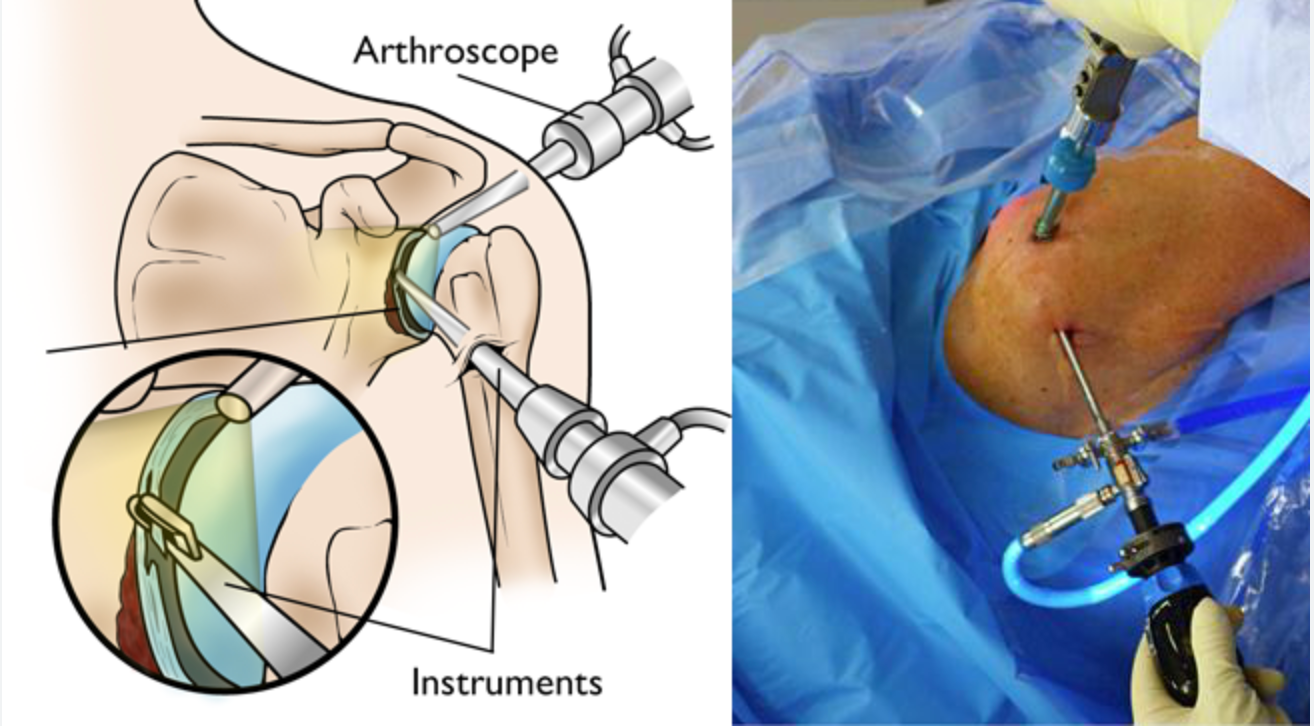
Shoulder arthroscopy is a minimally invasive procedure commonly used to visualize, diagnose, and treat various shoulder joint issues, including those affecting the rotator cuff. The surgeon begins by creating small portals, akin to tiny keyholes, around the shoulder joint. Through these portals, an arthroscope—a small telescope equipped with a light source and video camera—is inserted to provide a clear view inside the joint. Additional portals may be made as necessary, through which specialized instruments are inserted for various surgical tasks. The images captured by the arthroscope are displayed on a large screen monitor, enabling the surgeon to assess and address multiple shoulder problems with precision under arthroscopic guidance. Furthermore, images of shoulder pathologies and surgical videos can be recorded for documentation purposes.
Shoulder arthroscopy, being minimally invasive, presents several advantages: Smaller, cosmetically pleasing scars Reduced tissue injury Minimal pain Decreased swelling Shorter hospital stays Quicker recovery Dynamic tissue assessment under tension or probing Enhanced visualization of specific pathologies compared to open surgery
The shoulder, being the most mobile joint in the body, relies on a complex arrangement of structures to maintain stability during its wide range of movements. However, excessive mobility can increase the risk of injury and compromise shoulder stability. The glenoid, or shoulder socket, is notably flat, making it inherently unstable. To compensate, the glenoid is surrounded by a fibrous cartilage rim known as the labrum, which deepens the socket and provides some stability. Additionally, ligaments called capsular thickenings reinforce this stability. The long head of the biceps tendon, resembling a cord-like structure, originates from the top of the glenoid. Its attachment seamlessly blends with that of the labrum, further contributing to shoulder stability.
The following conditions serve as contraindications for a partial knee replacement: Shoulder arthroscopy is performed on a well-informed patient with appropriate consent. The procedure is conducted under general anesthesia with interscalene block, determined by the anesthetist based on individual factors such as age and health status. Patients are positioned either in the beach chair (sitting) or lateral (side-lying with the arm in traction) position, chosen based on the surgical requirements and the surgeon's expertise. Following thorough scrubbing of the shoulder, the surgeon makes a small keyhole incision (portal) at the back of the shoulder joint, previously marked. An arthroscope, equipped with a light source and tiny video camera, is inserted through one of the portals to visualize the shoulder structures, displayed on a large video monitor. Sterile saline solution is injected into the shoulder to distend it, providing a clear view and creating space for maneuvering. The surgeon meticulously examines the shoulder joint to determine the cause of the issue, capturing detailed photo images for documentation. Additional portals are created as needed, through which surgical instruments like probes, scissors, shavers, or radiofrequency probes are inserted to address the identified problems. Procedures may include repairing torn labrum, SLAP lesions, biceps tenodesis or tenotomy, rotator cuff repairs, capsular release for frozen shoulder, removal of loose bodies or calcium deposits, synovectomy, subacromial bursectomy, subacromial decompression, microfractures, or fixation of certain fractures. Upon completion of the arthroscopy, the shoulder joint is inspected for bleeding or damage, which is controlled using radiofrequency devices. Normal saline irrigation is used to clear debris, followed by drainage. Incisions are closed with sutures or sterile tapes, covered with dressings, and compression bandages are applied. Patients are provided with a shoulder sling and moved to the recovery room for observation.
Most patients are discharged either the same day or the next day following shoulder arthroscopy. Recovery duration varies based on the procedure complexity, with simple procedures often leading to faster recovery than complex ones. Preoperative counseling typically outlines a recovery period of 2 to 6 weeks for simple procedures and 6 to 12 weeks for complex ones. Shoulder arthroscopy generally facilitates faster recovery compared to open shoulder surgery. Pain medications are prescribed for the first 3 to 5 days to manage discomfort, with subsequent usage only as needed. Ice packs are recommended 4 to 5 times daily for 1 to 2 weeks to alleviate swelling. Prior to discharge, patients receive instruction from a physiotherapist on simple shoulder pendulum exercises to continue at home for 2 to 4 weeks. For complex surgeries, ongoing physiotherapy may be necessary for up to 2 to 3 months, ensuring a successful and expedited recovery. Depending on the complexity of the surgery, patients may require a simple shoulder sling or specialized shoulder braces for 2 to 6 weeks post-surgery. Guidance is provided on sling care to prevent issues like sweating or itching that may affect wound healing. Surgical wounds are assessed 10 days post-surgery, with dressings and sutures, if present, removed during this visit.
Shoulder arthroscopy is generally considered a safe procedure with rare complications. Possible complications may include bleeding into the shoulder joint, infection, swelling, shoulder stiffness, bruising around the shoulder joint, and damage to surrounding nerves, blood vessels, joint cartilage, tendons, and ligaments. In rare cases, continuing shoulder problems may also occur.
Address
8/92, Sector 8, Ismailganj, Indira Nagar, Lucknow, Uttar Pradesh 226016
Monday to Friday
10am - 8pm
Appoinments
+91 - 8840223370