Shoulder instability refers to an abnormal looseness of the shoulder joint, leading to the displacement of the humeral head (ball) from the glenoid socket. Unlike normal physiological laxity, instability is a pathological condition. Subluxation denotes a minor form of instability where the shoulder ball partially slips out of the socket, while dislocation represents a more severe scenario where the shoulder completely dislocates from its socket. Instability can develop through traumatic or atraumatic means. Traumatic instability occurs when the ligaments holding the shoulder ball in place are stretched or torn due to trauma or overloading, compromising their stability throughout the shoulder's extensive range of motion. On the other hand, atraumatic instability arises from general joint laxity, gradually leading to shoulder instability. Acute shoulder dislocations can be triggered by various factors. Common causes of anterior dislocation include falls on an outstretched arm forced overhead, direct blows to the shoulder, or forced external rotation of the arm. Conversely, posterior dislocation can result from events such as epileptic seizure attacks or electrocution, which generate abnormal muscular forces around the shoulder. Understanding these differences in shoulder instability is crucial for determining the most appropriate treatment approach.
Patients typically report a history of trauma, often followed by sudden and intense shoulder pain, along with a sensation of the shoulder popping out of its socket. This is accompanied by difficulty in moving the arm. Additional complaints may include swelling, noticeable deformity, numbness, or weakness.
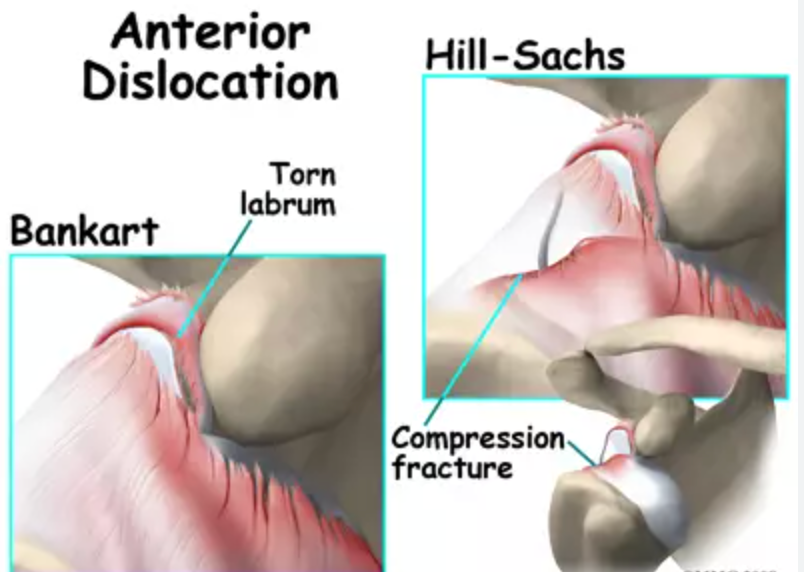
Diagnosing shoulder dislocation involves gathering information about the injury, conducting a thorough clinical examination, and performing X-rays. Patients typically exhibit immobility of the arm against the side due to pain, with any attempt to move the shoulder causing discomfort. Physical signs such as a prominent crease under the acromion and a bulge in the armpit provide clues to the direction of dislocation. Assessment includes testing range of motion, strength, and sensation, with changes indicating potential nerve damage. Additionally, the physician checks arm pulses to detect vascular complications. In cases of spontaneous relocation, diagnosis may be challenging, with patients describing the sensation of the shoulder "slipping out" before reduction. X-rays confirm the dislocation, its direction, and any associated fractures, such as a bony Bankart fracture indicating detachment of the labrum and ligaments from the glenoid. Arthroscopic remplissage procedure addresses engaging defects of the humeral head by tying down the infraspinatus tendon and posterior capsule, converting an infra-articular Hill-Sachs lesion into an extra-articular one, thereby preventing engagement with the glenoid rim during overhead activities. It's often combined with anterior Bankart repair to stabilize unstable shoulders and reduce recurrence. However, it carries the risk of limiting external rotation, making it unsuitable for patients requiring full external rotation for sports or occupational activities, such as throwers and fast bowlers.
Following clinical examination and X-rays confirming shoulder dislocation, the patient undergoes sedation or general anesthesia to relax the shoulder muscles. With assistance, the doctor applies gentle traction and manipulates the arm to realign the shoulder joint, known as closed reduction. Subsequent X-rays verify the successful relocation of the joint, providing immediate pain relief. A shoulder sling is prescribed for 2-4 weeks for support and comfort. Upon discharge, the patient is advised to seek follow-up with a Shoulder Specialist for further evaluation, including MRI and CT scans. Until the first follow-up, only gentle pendulum exercises are permitted.
Recurrent shoulder dislocations are most prevalent among young individuals, particularly athletes and those engaged in vigorous physical activities. The likelihood of recurrent instability increases with youth and activity level. For instance, if the initial dislocation happens during adolescence, there's a 70-90% probability of recurring instability. Conversely, individuals aged over 40 experiencing their first dislocation have less than a 10% risk of recurrent instability.
Chronic shoulder instability can arise from various factors: Traumatic shoulder dislocation: When the shoulder experiences a traumatic dislocation, the labrum, which helps deepen the socket, and the capsular ligaments, responsible for holding the shoulder ball in place, can sustain tears or stretching. This compromises the necessary stability of the ligaments across the shoulder's wide range of motion. Repetitive overhead activities: Engaging in repetitive overhead movements, common in sports like swimming, tennis, and volleyball, or certain occupational tasks, can lead to the gradual stretching of shoulder ligaments due to chronic overloading. With loosened ligaments unable to adequately support the humeral head within the socket, individuals may experience shoulder instability and pain during such activities. Multidirectional Instability: In a subset of patients, shoulder instability can occur without a history of injury or repetitive strain. These individuals may have naturally lax ligaments throughout their body, often referred to as being "double-jointed." As a result, the shoulder can dislocate in multiple directions, leading to a condition known as multidirectional instability (MDI). Some patients with MDI can voluntarily dislocate their shoulder without experiencing pain.
Common symptoms of chronic shoulder instability encompass pain resulting from shoulder injury, recurrent shoulder dislocations, frequent episodes of the shoulder giving out, and a persistent feeling of looseness or instability in the shoulder joint. Individuals experiencing chronic shoulder instability may also describe sensations of the shoulder slipping in and out of the joint or feeling as if it is "hanging there" without proper support. These symptoms often indicate underlying issues with the shoulder's structural stability and should prompt further evaluation by a healthcare professional.
After a comprehensive medical history review, the surgeon conducts a meticulous clinical examination to diagnose shoulder instability. Subsequent investigations, including X-rays and MRI scans, confirm underlying pathologies. X-rays reveal fractures such as the bony Bankart's lesion on the glenoid rim and impaction fractures like the Hill-Sachs lesion on the humeral head. MRI scans detect rotator cuff tears, biceps tendon lesions, and soft tissue Bankart's lesions involving labrum and capsular ligaments. CT scans may be required to assess glenoid bone loss. Treatment for shoulder instability is tailored based on factors like severity, patient age, activity level, and occupation. Dr. Niraj Ranjan Srivastava devises a treatment plan, whether conservative or surgical, considering all relevant factors. Initial treatment typically involves physiotherapy, activity modifications, and pain management. Strengthening exercises for the rotator cuff and periscapular muscles aim to stabilize the joint. Physiotherapy, customized for each patient, aids in regaining motion, reducing apprehension, and restoring shoulder function. Lifestyle adjustments and activity modifications are crucial to prevent repetitive stress on the shoulder and alleviate symptoms.
Surgery becomes a recommendation when recurrent instability persists despite sufficient physiotherapy and activity modification. It's advised particularly after the initial dislocation in young individuals under 20 years old, given their heightened risk of re-dislocation. Contact athletes intending to continue participating in sports that pose shoulder injury risks and individuals engaged in strenuous physical activities are also candidates for surgical intervention.
Shoulder stabilization surgery enhances patients' confidence, shoulder strength, and overall function by restoring stability. This enables them to resume normal work or sporting activities. Additionally, the surgery prevents further damage to the surfaces of the ball and socket caused by recurrent instability.
Shoulder instability surgery aims to restore the normal anatomy of the shoulder by repairing the torn cartilage ring (labrum) and re-tensioning the stretched capsular ligaments without excessive tightening. The goal is to regain stability in the shoulder while preserving as much motion as possible. This procedure, known as Bankart Repair, can be performed through either arthroscopic or open techniques. Depending on the extent of labral damage, typically 2 to 3 suture anchors (metallic or non-metallic) are placed at various locations on the glenoid rim (socket). Non-absorbable sutures attached to these anchors are then passed through the torn capsular labral tissue and tied from bottom to top to restore the labrum to its normal position. This reconstruction recreates the natural labral bumper effect and re-tensions the capsular ligaments. By the end of the procedure, the humeral head is re-centered over the glenoid, ensuring stability and mobility of the shoulder joint.
Arthroscopic shoulder stabilization, also known as Bankart Repair, utilizes a fiber-optic telescope, camera, and specialized instruments through 3 to 4 small incisions. Dr. Niraj Ranjan Srivastava specializes in these minimally invasive procedures for various types of shoulder instabilities and dislocations. Arthroscopic stabilization offers several advantages, including minimal scarring for improved cosmetic results, reduced tissue trauma and pain, decreased bleeding, shorter hospital stays, excellent visualization of the shoulder joint and associated instability lesions, simultaneous management of additional shoulder pathologies like rotator cuff tears or biceps tendon lesions, comparable success rates to open stabilization surgery, and faster recovery times.
The Latarjet procedure, also known as the Latarjet-Bristow procedure, is a surgical intervention utilized to address recurrent shoulder dislocations, often attributed to glenoid bone loss or fractures. Originating from the work of French surgeon Dr. Michel Latarjet in 1954, this procedure is conducted through either open or arthroscopic techniques, particularly for patients exhibiting more than 15 to 20% glenoid bone loss, as confirmed by CT scans. It involves the extraction and relocation of a portion of the coracoid process, along with its attached tendons, to the anterior aspect of the glenoid. This bone block is secured flush to the lower glenoid region using specialized screws, thereby filling the void caused by recurrent dislocations and augmenting glenoid width. The mechanism of action of the Latarjet procedure is often described as a Triple Blocking Effect, which stabilizes the shoulder and mitigates further dislocations by: 1) Increasing or restoring the width of the glenoid bone; 2) Creating a sling effect of the Conjoint tendon on the subscapularis and capsule, particularly in the abducted and externally rotated arm position where dislocations commonly occur; and 3) Repairing the capsule to the stump of the coracoacromial ligament to re-tension the capsules and provide stability against dislocations. The Latarjet procedure is deemed the preferred shoulder reconstruction method for various individuals, including contact athletes, patients with increased shoulder laxity, those with failed previous reconstructions, and individuals with significant bone damage to the glenoid and humeral head. It offers the advantage of maintaining external rotation movement and facilitating participation in sporting activities. With careful patient selection, the Latarjet procedure demonstrates high efficacy, preventing recurrent anterior instability in approximately 94-99% of cases.
Remplissage, a French term meaning 'to fill-in', refers to an arthroscopic shoulder surgery aimed at addressing recurrent anterior shoulder dislocations in patients with a substantial engaging Hill-Sachs defect of the humeral head coupled with a Bankart lesion of the glenoid. These individuals often present with unstable shoulders, particularly experiencing dislocations when the arm is abducted and externally rotated, causing the Hill-Sachs lesion to catch against the anterior rim of the glenoid. Dr. Niraj Ranjan Srivastava, an experienced orthopedic surgeon specializing in joint replacement and arthroscopy, performs this procedure to restore shoulder stability and mitigate recurrent dislocations.
Open shoulder stabilization is beneficial under the following circumstances: When there is a concurrent fracture of the socket (glenoid) or humeral head. In cases where the glenoid has worn out, assuming an inverted pear shape due to recurrent anterior instability. Following failure of prior shoulder stabilization surgeries. When the surgeon lacks experience in arthroscopic stabilization techniques. When capsular tissue is deemed irreparable and requires the transfer of a bony block with attached soft tissues, such as in the Latarjet procedure, or an iliac crest bone block transfer.
Address
8/92, Sector 8, Ismailganj, Indira Nagar, Lucknow, Uttar Pradesh 226016
Monday to Friday
10am - 8pm
Appoinments
+91 - 8840223370