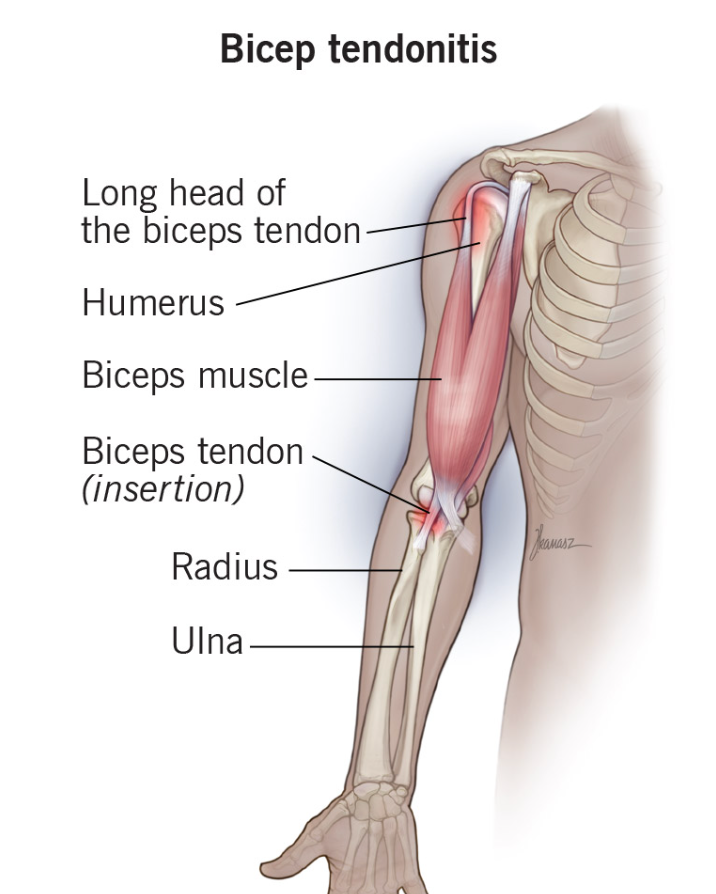
The biceps tendon is a lengthy cord-like structure situated at the front of the shoulder. It originates from the top of the glenoid, or shoulder socket, and traverses the joint via the biceps groove, a bony trough. Below the shoulder, it transforms into the long head of the biceps muscle. The short head of the biceps is an extension of the conjoined tendon, originating from the coracoid, a bony projection at the front of the shoulder blade. In the shoulder region, the biceps muscle has two attachment points and plays a crucial role in flexing (bending) the elbow and rotating the forearm.
Biceps tendon injuries are frequently encountered in particular age groups. With the passage of time, tendons lose their elasticity, becoming stiffer and more prone to brittleness. Furthermore, the blood supply to the tendon diminishes with increasing age, exacerbating the degenerative process, particularly in sedentary individuals. However, engaging in proper and regular exercises can mitigate this degeneration to some extent. Nevertheless, even well-trained individuals and athletes are susceptible to biceps tendon injuries. Despite being in good health, tendons can still sustain damage from overuse and excessive training.
The biceps tendon can weaken due to aging, inactivity, or excessive activity, making it more susceptible to injuries. Reduced tolerance to repetitive actions and sudden loads increases the risk of injury. Some patients may develop bone spurs in the bicipital grooves or beneath the acromion, the top of the shoulder blade. These bone spurs can cause friction against the tendon, leading to wear and tear. Dislocation of the biceps tendon from its groove is observed in some patients, often in conjunction with a tear of the subscapularis or rotator cuff tendons, which normally help stabilize the biceps tendon. Additionally, injuries can occur at the attachment site of the biceps tendon on top of the glenoid, often involving avulsion, where the tendon is pulled off the bone, rendering it unstable.
Irritation of the biceps tendon or its sheath can lead to tendon inflammation, resulting in pain and swelling, a condition known as tendinitis. Mild injuries may cause microscopic tearing of individual tendon fibers, while more severe injuries can result in larger tears or even partial or complete ruptures of the biceps tendon. In cases of complete rupture, the long head of the biceps tendon typically descends towards the elbow, yet bicep muscle function usually remains nearly normal due to its dual attachment proximally. Diagnosing biceps tendon problems involves a comprehensive approach, including the patient's medical history, thorough clinical examination, and appropriate investigations. Patients typically report pain in the front of the shoulder, particularly during overhead activities or lifting. Tenderness is often present upon probing the front of the shoulder, along with pain during specific shoulder movements. Associated shoulder weakness may indicate inflammation or tears in the rotator cuff tendons. Complete rupture of the biceps tendon can be identified by a visible and palpable lump in the arm, especially when bending the elbow (known as the "pop-eye sign"). Shoulder x-rays are useful for detecting any bony spurs at the acromion or in the bicipital groove.
Initially, rest, ice packs, and anti-inflammatory medications are essential for managing symptoms. If pain persists, a steroid injection may be necessary to alleviate pain and reduce swelling. In severe cases where conservative measures fail to yield improvement, arthroscopic surgery may be indicated.
The choice of surgical treatment for biceps tendon injuries depends on the severity and extent of the damage. For minor tendon damage, a simple arthroscopic debridement may suffice, which involves shaving off the torn fibers to alleviate pain and restore function. In cases where a significant portion of the tendon is affected, a biceps tenodesis procedure is recommended. This surgery involves relocating the biceps tendon from its original attachment point on the top of the glenoid to the upper humerus using specialized devices such as suture anchors or screws. This allows the tendon to heal at its new location while maintaining the functional length of the biceps muscle, resulting in reduced pain and restored shoulder function. Younger patients typically benefit the most from this procedure. If the biceps tendon is completely ruptured, particularly causing the characteristic bulging appearance in the upper arm (pop-eye sign), a biceps tenodesis procedure is also performed, especially in younger patients. However, successful re-attachment depends on the visibility and traceability of the tendon's upper end. In cases where the tendon cannot be re-attached, such as when it slides too far distally or in delayed presentations where the tendon is scarred and immobile, a biceps tenotomy may be performed. This involves cutting the tendon from its attachment site, allowing the tendon end to slide down. While this procedure can alleviate shoulder pain and improve function, it may result in a cosmetic deformity known as the pop-eye sign, particularly in elderly patients who may undergo this procedure due to significant tendinitis and fraying of the biceps tendon. If the tendon is partially avulsed from its origin on the top of the glenoid along with the labrum (SLAP lesion), it may be repaired arthroscopically using tiny suture anchors in a procedure known as SLAP Repair.
Following biceps tendon surgery, patients undergo a structured recovery process. Typically, they are discharged either on the same day or the following day post-surgery. A shoulder sling is provided for 3 to 4 weeks to provide support during the initial healing phase. Pain management is facilitated with painkillers and anti-inflammatory medications taken as needed, while ice packs are applied multiple times daily to alleviate swelling and discomfort. Patients can gradually resume desk-type work after 1 to 2 weeks, accompanied by the initiation of gentle shoulder pendulum exercises performed 2 to 3 times daily. Physiotherapy sessions, typically spanning 2 to 3 months, aid in rehabilitation. Tendon healing usually takes 6 to 8 weeks, allowing for the gradual reintroduction of overhead activities after 6 weeks. However, heavy lifting should be avoided for 3 months. Patients can gradually return to unrestricted activities, including work and sports, after completing approximately 3 to 4 months of dedicated shoulder rehabilitation.
Address
8/92, Sector 8, Ismailganj, Indira Nagar, Lucknow, Uttar Pradesh 226016
Monday to Friday
10am - 8pm
Appoinments
+91 - 8840223370