The Anterior Cruciate Ligament (ACL) serves as a key stabilizing ligament within the knee. Positioned centrally, it extends from the back of the femur to the front of the tibia. Its primary role is to prevent excessive forward movement of the tibia, thereby maintaining knee stability, particularly during rotational movements such as twisting, turning, or side-stepping activities. Additionally, the ACL contributes to providing essential neurological feedback regarding limb orientation, which is crucial for normal joint function during daily activities, occupational tasks, and sports.
Injuries to the ACL commonly occur in contact sports such as football, as well as in pivoting sports like skiing. Non-contact movements such as side-stepping, pivoting, or landing from a jump can also lead to ACL tears. Additionally, sudden twisting of the knee, as may happen in motorbike or car accidents, can result in ACL injury
In the acute phase: Sensation or sound of a pop during ACL injury Swelling of the knee Knee pain Difficulty bearing weight or walking Difficulty bending the knee In chronic stages: Sensation of knee giving way and instability with twisting movements Pain Swelling
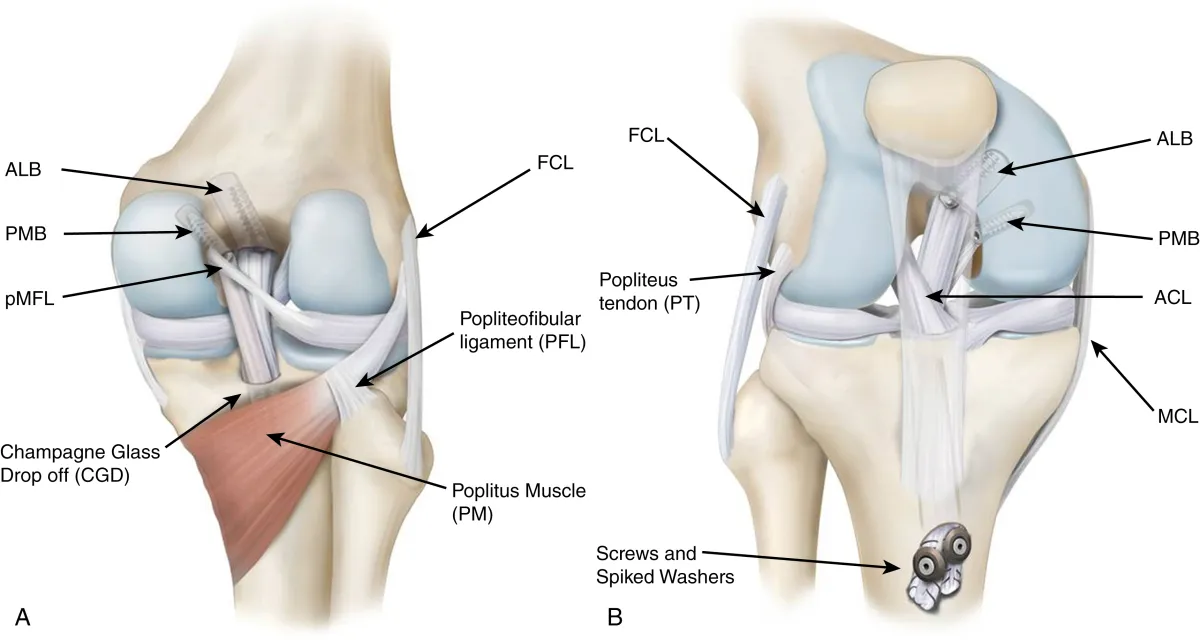
Injuries to other structures around the knee joint can include: Meniscal injuries: Damage to the outer (lateral) or inner (medial) meniscus, or both. Cartilage injuries: Damage to the cartilage lining the femur, tibia, or patella, ranging from minor flaps to major defects. Ligament injuries: Injuries to the medial collateral (MCL), lateral collateral (LCL), or posterior cruciate (PCL) ligaments. Fractures: Fractures involving the tibia or femur.
Diagnosing an ACL injury typically relies on the patient's injury history, symptoms, and clinical examination. Special tests are conducted to confirm excessive forward movement and tibial pivoting. However, in acute cases where clinical examination is hindered by pain and swelling, MRI is often employed to confirm the diagnosis. While a torn ACL is not visible on x-rays, they can reveal fractures around the knee joint, particularly avulsion of the tibial spine where the ACL attaches to the shinbone
The various types of ACL injuries are categorized as follows: Grade I: Involves mild stretching of the ACL fibers with some micro-tearing, resulting in no instability of the knee. Grade II: Indicates severe stretching of the ACL fibers with incomplete (partial) tears of the ligament, leading to moderate knee instability during strenuous activities. Grade III: Characterized by complete tearing of the ACL fibers, rendering the ligament unable to provide stability to the knee joint. ACL avulsion fracture: This unique ACL injury occurs when the bony attachment of the ACL at the tibia is pulled off from the upper tibia. In this scenario, the ACL fibers remain intact. This injury is also referred to as a tibial spine fracture and can involve either undisplaced or displaced fragments.
Not all patients with an ACL injury require surgery. You may opt out of surgery if you: Have a minor tear in your ACL that can heal with rest and rehabilitation. Are not highly active in sports, and your occupation does not necessitate a stable knee. Are willing to discontinue activities that demand a stable knee or perform them at a reduced intensity level. You may choose alternative activities like cycling or swimming. Can commit to a rehabilitation program that stabilizes your knee and strengthens your leg muscles to lower the risk of future knee injuries and are comfortable with a slight degree of knee instability. Lack the motivation to undergo the extensive and demanding rehabilitation program required post-surgery.
Conservative treatment for an ACL injury involves several approaches aimed at promoting healing and improving knee stability: Rest: Avoiding sports or heavy work to allow the knee to recover. Ice pack: Applying ice to reduce swelling and alleviate pain. Anti-inflammatory medications: Using medication to reduce pain and inflammation. Physiotherapy: Engaging in exercises to strengthen the muscles around the knee, particularly the hamstrings, which can compensate for the role of the ACL in knee stability. Balance and proprioception training: Performing specific exercises to retrain nerves and compensate for the loss of ACL function in providing information about knee joint position. Functional Knee Braces: These may be prescribed to aid patients with damaged ACLs, although their benefits are not fully understood. While they may assist with proprioception, they are costly and may not offer significant support to knee stability.
Conservative treatment for an ACL injury involves several approaches aimed at promoting healing and improving knee stability: ACL reconstruction is typically recommended for individuals who have experienced a complete tear or significant partial tear of the ACL, resulting in instability of the knee joint. In cases where rehabilitation efforts have proven ineffective in restoring stability, or for those engaged in sports or occupations that demand strong and stable knees, surgery may be advised to regain pre-injury levels of function. Commitment to a rigorous and lengthy rehabilitation program is essential for successful outcomes. Additionally, individuals experiencing chronic ACL deficiency that impairs their quality of life, or those with accompanying injuries such as displaced ACL avulsion fractures or damage to other knee structures like cartilage, meniscus, ligaments, may also benefit from ACL reconstruction surgery.
A torn ACL leads to abnormal tibial mobility during everyday activities and sports, causing secondary damage to joint cartilage and meniscal tissues. This damage often accelerates the onset of knee arthritis, restricting patients from engaging in active sports or maintaining a vigorous lifestyle due to instability and fear of knee buckling. For active athletes, an ACL injury can be career-threatening. The primary goal of ACL surgery is to restore normal or near-normal stability in the knee, aiming to return patients to their pre-injury level of function while minimizing loss of knee function, preventing further injury and degeneration of knee structures like articular cartilage and menisci, and enabling patients to resume an active lifestyle encompassing sports and recreational activities.
The selection of surgical procedures for treating various types of ACL injuries relies on several factors, including the nature of the ACL injury, the condition of any remaining ACL remnants or stumps, and the duration since the injury occurred. Surgeons base their decisions on arthroscopic evaluations of ACL tears and their characteristics. Among the options available, arthroscopic ACL reconstruction has long been considered the standard, involving the replacement of the torn ACL with graft tissue. However, arthroscopic augmented ACL reconstruction is rapidly gaining popularity, as it reinforces the reconstructed ACL with additional graft material or synthetic devices. In specific cases, surgeons may opt for arthroscopic primary repair of the ACL tear, typically for patients with proximal tears and adequate tissue quality and blood supply. Alternatively, they may perform arthroscopic primary ACL repair with augmentation, combining primary repair with additional graft material or synthetic devices to bolster stability. Ultimately, the choice of surgery is tailored to each patient's unique circumstances, aiming to restore knee function and stability effectively.
ACL reconstruction surgery aims to restore the stabilizing function of the injured anterior cruciate ligament (ACL), which is the most common ligament reconstruction procedure performed around the knee joint. This procedure involves removing the damaged ACL remnants and replacing them with another soft tissue, known as a graft. Autografts, sourced from the patient's own body, are the most commonly used grafts, often harvested from the same side requiring reconstruction or, in some cases, from the opposite knee in multi-ligament or revision ACL surgeries. Allografts, harvested from cadavers and processed for patient use, are occasionally utilized in specific cases. The two primary graft techniques involve using hamstring tendons or patellar tendon grafts, also known as Patellar Tendon Bone (PTB) or Bone Tendon Bone (BTB) grafts, which consist of a central strip of patellar tendon with bony plugs at each end. Surgeons may also employ Quadriceps Tendon Bone (QTB) grafts from the front of the lower thigh or entirely soft tissue grafts like the Peroneus Longus Tendon (PLT) from the outer side of the ankle. ACL reconstruction surgery can be performed through open techniques or arthroscopically, utilizing telescopes, cameras, and specialized instruments. Arthroscopy offers benefits such as excellent visualization of knee joint structures, minimal scarring for better cosmetic results, reduced tissue damage and bleeding, decreased postoperative pain, shorter hospital stays, and faster rehabilitation.
Patients undergoing ACL surgery for appropriate indications and adhering to rehabilitation protocols typically achieve a 90 to 95% success rate. Successful outcomes are characterized by restored muscle strength, knee stability, and pain-free range of motion. Such patients can resume their pre-injury occupations or sports activities after completing a rehabilitation program lasting at least 6 to 9 months.
During ACL surgery, the patient is typically under general, spinal, or epidural anesthesia, and a tourniquet is applied to the upper thigh to create a bloodless surgical field. A telescope with a camera and light source is inserted into the knee joint through small portals on either side of the lower portion of the patella. Diagnostic arthroscopy is conducted to assess all structures within the knee joint, addressing any meniscal or cartilage injuries first. Once the ACL tear is confirmed and its type noted, the remnants of the torn ACL are evaluated. Depending on their quality, they may be cleared with a shaver from their attachments on the femur and tibia. Sites for inserting the new ACL at the tibial and femoral ends are identified, and hamstring tendon grafts are harvested through a small incision on the upper part of the leg. The graft is prepared, marked for length, and then pulled into the knee joint through drilled bone tunnels. Fixation of the graft at the femur side is achieved with an endo-button or screw, while fixation at the tibial side is done with a screw. The new ACL is checked for position, tension, fixation strength, and any signs of impingement throughout the knee's range of motion. Finally, wounds are sutured or closed with sterile tapes, dressed, and a compression bandage is applied, along with a hinged knee brace.
Augmented ACL Reconstruction is a surgical technique wherein the torn or damaged portions of the native ligaments are preserved or minimally trimmed while simultaneously reconstructing a new ACL using a tendon graft. The approach offers several principles and advantages: 1. Preservation of ACL stumps (remnants) serves as definitive landmarks for creating femoral and tibial tunnels precisely, facilitating anatomical ACL reconstruction. 2. ACL remnants aid in re-vascularization and healing of the new graft, accelerating the graft healing and maturation processes. 3. The presence of ACL remnants promotes the regrowth of nerves within the graft, enhancing joint sense and providing knee stability, particularly during the early phases of graft healing. This results in faster rehabilitation and better functional recovery, with lower rates of graft re-rupture. 4. Specialized and strong suture materials can be utilized to augment the autograft, enhancing its mechanical strength. This augmentation provides early strength and protection to the new graft during the healing process, allowing for faster rehabilitation. 5. Biologic augmentation aims to expedite scar tissue healing within the bony tunnels and facilitate faster graft healing. Platelet-rich plasma (PRP), derived from the patient's own blood, is commonly used for this purpose, although its long-term effects are still being studied.
Yes, it's indeed possible to repair a torn ACL in specific patient groups, showing promising outcomes. Experienced surgeons can perform this procedure across all age groups for suitable candidates. The success of ACL repair is attributed to advancements in understanding native ACL anatomy and biomechanics, along with improvements in fixation implants and techniques. Primary ACL repair involves reattaching the ACL stump to the femur bone using specialized sutures and implants, facilitating healing and preserving the native ACL anatomy with its functional advantages. This approach is indicated in proximal ACL tears with good tissue quality, cases where the ACL stump is attached to the PCL, isolated ACL injuries, pediatric patients to avoid growth plate injury, and multi-ligament knee injuries. Primary ACL repair offers several advantages: Avoidance of graft harvesting Preservation of native ligament biology and blood supply Near-normal knee kinematics Potential for fast-tracked rehabilitation and early return to sports Slowing down the progression of knee arthritis compared to ACL reconstruction Tissue tape augmentation in primary ACL repair enhances stability during the repair process, protecting the ligament from necrosis and promoting faster healing. This augmented repair construct is biomechanically superior to non-augmented repair techniques.
Your hospital stay will be 1-2 days
Patients typically begin walking or moving their knee on the same day or the day after the operation. Initially, they may require assistance from elbow crutches or a walker for mobilization. Detailed instructions regarding specific exercises for the next three months will be provided, with weekly monitoring by our physiotherapist to ensure progress. Our team will provide guidance and support throughout your recovery period.
I recommend continuing physiotherapy for a minimum of three months to restore normal knee motion, achieve good muscle strength, and enhance stability (proprioception) in the knee joint. Following this initial phase, patients are encouraged to continue rehabilitation for an additional six to nine months in a progressive manner to maximize the benefits of ACL reconstruction. During the first three months, soft tissue graft healing occurs within the bony tunnels of the tibia and femur. At this stage, the graft is weakest as it undergoes structural remodeling. Over the subsequent six to nine months, the graft gradually strengthens, reaching its original strength around nine to twelve months post-surgery. This process, known as graft ligamentization, necessitates regular physiotherapy to incrementally advance patients' workout intensity based on their strength improvement and time elapsed since surgery. Patients who fully adhere to the rehabilitation program have a high likelihood of success. Their knee stability is restored, mobility is fully regained, and they can resume most normal activities, including sports. However, attempting high-intensity activities or sports before the graft has completed its healing and strengthening process (before nine months) significantly increases the risk of graft rupture. Therefore, we extensively counsel ACL reconstruction patients about the gradual healing and strengthening of the new graft over an extended period to ensure optimal outcomes.
The duration of crutch use will vary based on your individual progress, typically ranging from 2 to 4 weeks.
The duration of knee brace usage will be determined by your progress, typically ranging from 4 to 6 weeks.
Sutures are typically removed 10 to 12 days post-surgery.
For office-type jobs, you can typically return to work after 1 to 2 weeks, while for other heavy-intensity jobs, return to work may be possible after 3 months, contingent upon satisfactory progress.
You can resume driving a car after 4 to 6 weeks and riding a motorbike after 6 to 8 weeks, given that your knee is pain-free and exhibits good range of motion, strength, and stability.
In general, participation in any sporting activities is restricted for 6 to 9 months following ACL reconstruction surgery. Full intensity sports are typically permitted after completing 9 months of rehabilitation.
ACL Reconstruction, like any surgical procedure, entails inherent risks. These include potential allergic reactions to anesthesia medications and breathing difficulties during the procedure. Additionally, general surgical risks such as bleeding and infection are present. Specific to ACL reconstruction, patients may experience post-operative complications such as knee stiffness, failure of ligament healing, or malfunction of graft fixation devices. Knee pain and weakness are possible, as are blood clots in the leg and injury to nearby blood vessels, nerves, or tendons. Numbness on the outer side of the knee, difficulty kneeling, and even patellar fractures in cases of patellar tendon graft usage can occur. Moreover, there's a risk of ligament rupture if the knee suffers further injury post-surgery. Despite these risks, ACL reconstruction is generally considered a safe and effective procedure for restoring knee stability and function.
Address
8/92, Sector 8, Ismailganj, Indira Nagar, Lucknow, Uttar Pradesh 226016
Monday to Friday
10am - 8pm
Appoinments
+91 - 8840223370