Shoulder joint arthritis occurs when the smooth cartilage within the joint deteriorates over time. This degeneration can lead to pain, stiffness, and limited mobility in the shoulder. When conservative treatments fail to provide relief, surgical options may be considered, including joint replacement or arthroscopy. One common surgical intervention for shoulder arthritis is total shoulder replacement, where damaged joint surfaces are replaced with artificial components. Another approach, known as reverse total shoulder replacement, is utilized for specific conditions such as completely torn rotator cuffs combined with severe arthritis (cuff tear arthropathy), failed previous shoulder replacements or fractures, particularly of the upper humerus. In reverse total shoulder replacement, the traditional positions of the ball and socket are reversed. The ball component is fixed to the shoulder blade at the glenoid and remains stationary, while the socket is attached to a stem inserted into the upper end of the humerus bone and remains mobile. This surgical technique relies on the intact deltoid muscle for shoulder movements.
Common causes of shoulder arthritis include: Osteoarthritis: This degenerative condition, often referred to as 'wear-and-tear' arthritis, damages the smooth outer covering (articular cartilage) of bone. It predominantly affects individuals over 50 years old and is more prevalent in the acromioclavicular joint than in the glenohumeral shoulder joint. Rheumatoid Arthritis: Rheumatoid arthritis is an autoimmune systemic inflammatory disorder affecting the synovium, or joint lining. It can occur at any age and typically involves multiple joints on both sides of the body. Post-traumatic Arthritis: This form of arthritis develops following an injury, such as a fracture or dislocation of the shoulder. Arthritis may also arise after a rotator cuff tear. Avascular Necrosis (AVN): AVN occurs when the bone of the humeral head dies due to a lack of blood supply. Risk factors for AVN include chronic steroid use, deep-sea diving, severe shoulder fractures, sickle cell disease, and heavy alcohol consumption.
Symptoms of shoulder arthritis typically include joint pain, stiffness, and weakness. Pain in the shoulder joint is a common complaint, exacerbated by activity and often worsening over time. When the glenohumeral joint is affected, the pain tends to localize to the back of the shoulder and may intensify with changes in weather conditions. Stiffness or limited motion is another prevalent symptom. Activities such as lifting your arm to comb your hair or reaching up to a shelf may become increasingly challenging. Additionally, you may notice a clicking or snapping sound (crepitus) when moving your shoulder, and weakness in the shoulder muscles may be present. As the condition progresses, any movement of the shoulder can elicit pain. Night pain is frequently reported, leading to difficulty sleeping. These symptoms collectively indicate the presence and progression of shoulder arthritis.
The diagnosis of shoulder arthritis relies on patient symptoms, a comprehensive medical history, thorough clinical examination, and appropriate investigations. Clinical assessment involves evaluating various factors, including muscle weakness (atrophy), tenderness upon palpation, and the extent of both passive (assisted) and active (self-directed) range of motion. Additionally, signs of injury to the surrounding muscles, tendons, and ligaments are examined, along with any indications of prior injuries. Presence of symptoms in other joints may suggest conditions like rheumatoid arthritis. Crepitus, a grating sensation within the joint during movement, and pain elicited by pressure on the joint are also assessed. X-rays of an arthritic shoulder typically reveal narrowing of the joint space, bone changes, and the formation of bone spurs (osteophytes). Complementary imaging techniques such as CT and MRI scans are utilized to assess the severity of bony deformities, extent of bone loss, and the condition of soft tissues, particularly the rotator cuff. Furthermore, if a local anesthetic injection into the joint provides temporary pain relief, it supports the diagnosis of shoulder arthritis. These diagnostic approaches collectively aid in accurately identifying and understanding the extent of shoulder arthritis.
The initial treatment approach for shoulder arthritis is typically non-surgical and may involve physiotherapy along with various self-care measures: Rest or activity modification: Adjusting activities to avoid exacerbating pain and modifying arm movements may be necessary to alleviate discomfort. Physiotherapy: Engaging in physiotherapy exercises, particularly in the early stages of arthritis, can help maintain joint mobility and strengthen the shoulder muscles. Application of moist heat: Moist heat application can provide relief by relaxing the muscles and reducing stiffness in the shoulder joint. Anti-inflammatory and pain medications: Over-the-counter medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or analgesics may be recommended to alleviate pain and inflammation. Ice therapy: Applying ice to the shoulder for 20 minutes, two to three times a day, can help reduce inflammation and relieve pain. For individuals with rheumatoid arthritis, disease-modifying drugs like methotrexate may be prescribed by the doctor, or a series of corticosteroid injections may be recommended to manage inflammation and pain effectively. These treatments aim to alleviate symptoms and improve the overall function of the shoulder joint affected by arthritis.
Shoulder arthroscopy surgery is typically considered most effective in the early stages of arthritis. During this procedure, the surgeon aims to alleviate symptoms by trimming the inflamed synovial lining tissue and removing debris and degenerated cartilage fragments from the joint. While this surgery can provide temporary relief from symptoms, it's essential for patients to understand that arthroscopic surgery does not cure arthritis, and the benefits derived from the procedure may not be permanent. Therefore, patients should be counseled regarding the limitations of the surgery and the potential for symptom recurrence over time.
Shoulder replacement surgery is typically recommended under the following circumstances: Persistent moderate to severe shoulder pain significantly impacting daily activities. Lack of improvement in pain despite regular use of pain medications. Adverse effects experienced from pain medication usage. Minimal pain relief even after modifying or restricting activities. Ineffectiveness of physiotherapy in alleviating symptoms. X-ray confirmation of advanced shoulder (glenohumeral) arthritis. Previous unsuccessful surgeries such as failed fracture fixation or revision (re-do) shoulder replacement necessitating further intervention.
Shoulder replacement is contraindicated in cases of: Active or recent infection in the shoulder joint. Paralysis of deltoid or rotator cuff muscles. Neuropathic joint (Charcot joint). Glenoid resurfacing is not recommended for massive rotator cuff tears that are deemed non-repairable.
Shoulder replacement surgery entails replacing the painful surfaces of the damaged shoulder with artificial components. Typically, the ball part of the shoulder joint is replaced with a stem featuring a rounded, highly polished metal head. Meanwhile, the socket part is substituted with a durable, smooth plastic concave shell that complements the round head of the ball.
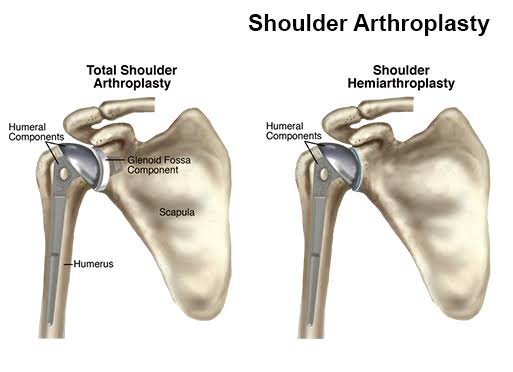
There are various types of shoulder replacements: Shoulder Hemiarthroplasty: This involves the partial replacement of the shoulder, where only the humeral head (ball part) is replaced. If the glenoid (socket) has good cartilage, it is not replaced. Sometimes, the decision to perform a total shoulder arthroplasty or hemiarthroplasty is made during the surgery itself.
Shoulder Hemiarthroplasty: This involves the partial replacement of the shoulder, where only the humeral head (ball part) is replaced. If the glenoid (socket) has good cartilage, it is not replaced. Sometimes, the decision to perform a total shoulder arthroplasty or hemiarthroplasty is made during the surgery itself.
 Total Shoulder Replacement: This procedure entails replacing the arthritic joint surfaces with a ball attached to a stem and a plastic socket. Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are often suitable candidates for conventional total shoulder replacement.
Total Shoulder Replacement: This procedure entails replacing the arthritic joint surfaces with a ball attached to a stem and a plastic socket. Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are often suitable candidates for conventional total shoulder replacement.
The shoulder replacement components are available in various types and sizes. If the bone quality is good, the surgeon may opt for a non-cemented or press-fit humeral component. These implants feature a special porous coating that allows bone to grow into them, providing lasting stability.
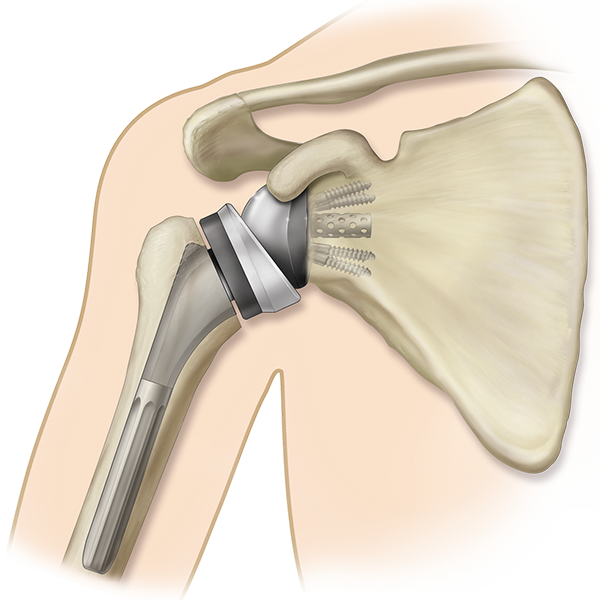
 Reserved Shoulder Replacement: Reverse shoulder replacement is a type of shoulder replacement where the natural ball and socket configuration of the glenohumeral joint is reversed, resulting in a more stable joint with a fixed fulcrum. This approach is used in cases where conventional shoulder replacement surgery would likely result in poor outcomes and high failure rates.
Reserved Shoulder Replacement: Reverse shoulder replacement is a type of shoulder replacement where the natural ball and socket configuration of the glenohumeral joint is reversed, resulting in a more stable joint with a fixed fulcrum. This approach is used in cases where conventional shoulder replacement surgery would likely result in poor outcomes and high failure rates.
Shoulder resurfacing surgery offers an alternative to traditional shoulder replacement for addressing shoulder arthritis, providing a bone-conserving approach known as hemi-arthroplasty.
In this procedure, instead of replacing the entire joint, only the damaged ball of the shoulder joint is addressed. The surgery involves removing the damaged cartilage from the head of the humerus, along with a minimal amount of normal bone from the humerus neck.
Following the removal of damaged tissue, a metallic cap is fitted onto the humeral head. This cap may be secured with bone cement or be uncemented, featuring a special coating on its inner side to encourage bony ingrowth for stability and fixation.
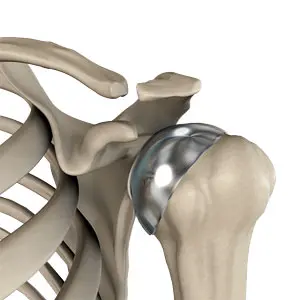
Shoulder resurfacing surgery offers an alternative to traditional shoulder replacement for addressing shoulder arthritis, providing a bone-conserving approach known as hemi-arthroplasty. In this procedure, instead of replacing the entire joint, only the damaged ball of the shoulder joint is addressed. The surgery involves removing the damaged cartilage from the head of the humerus, along with a minimal amount of normal bone from the humerus neck. Following the removal of damaged tissue, a metallic cap is fitted onto the humeral head. This cap may be secured with bone cement or be uncemented, featuring a special coating on its inner side to encourage bony ingrowth for stability and fixation.
Total shoulder replacement is highly successful, with a success rate of approximately 95% in pain relief, comparable to that of total hip or knee replacement surgeries. Following shoulder joint replacement surgery, patients experience a significant improvement in their quality of life. Pain is either eliminated or substantially reduced, and they enjoy enhanced motion, increased strength, and improved overall function.
Shoulder replacement surgery carries certain risks, including: Stiffness Infection Axillary nerve injury, which typically resolves as neuropraxia Peri-prosthetic fractures Rotator cuff tears Glenoid loosening Instability
Following shoulder replacement surgery, patients undergo a carefully monitored recovery process aimed at restoring shoulder function and strength. Initially, patients are hospitalized for a brief period, typically 1 to 2 days, and then provided with a shoulder sling for support and comfort. Over the next 6 weeks, the sling remains in place to facilitate soft tissue healing. During this time, patients engage in gentle exercises, such as pendulum movements and passive assisted exercises, to promote healing without stiffness. Wound healing is monitored, and sutures are removed around the 10-day mark post-surgery. From the 6th to 12th weeks, patients gradually regain range of motion through active exercises. Beyond the 12-week mark, focus shifts to strength training under the guidance of a physiotherapist, with the aim of improving shoulder muscle strength. This comprehensive rehabilitation program typically continues for 6 to 12 months post-operatively to ensure the optimal outcome of the shoulder replacement surgery
Address
8/92, Sector 8, Ismailganj, Indira Nagar, Lucknow, Uttar Pradesh 226016
Monday to Friday
10am - 8pm
Appoinments
+91 - 8840223370